Heparin Drip Calculation Ml Hr
The heparin drip is a commonly used method in medical settings to administer anticoagulant medication, heparin, to patients. It is a crucial aspect of managing certain medical conditions, particularly those involving blood clotting disorders or during surgical procedures. Accurate calculation and administration of the heparin drip dosage are essential to ensure patient safety and optimal therapeutic outcomes.
In this comprehensive guide, we will delve into the world of heparin drip calculations, focusing on the specific unit of ml/hr (milliliters per hour). We will explore the factors that influence heparin dosage, provide step-by-step instructions for calculating the drip rate, offer real-world examples, and discuss the importance of individualized patient care. Additionally, we will examine the potential risks and considerations associated with heparin therapy and highlight best practices for healthcare professionals to ensure safe and effective administration.
Understanding Heparin and Its Therapeutic Uses

Heparin, a naturally occurring anticoagulant, plays a vital role in preventing and treating blood clots in various medical scenarios. Its mechanism of action involves inhibiting certain clotting factors, thus reducing the likelihood of thrombosis and embolism.
Medical professionals utilize heparin in a variety of settings, including but not limited to:
- Surgery: Heparin is commonly administered pre- and post-surgery to prevent clot formation, especially in patients undergoing procedures with a high risk of blood clotting.
- Cardiovascular Diseases: Patients with conditions like atrial fibrillation, deep vein thrombosis (DVT), or pulmonary embolism may require heparin therapy to manage their anticoagulation needs.
- Dialysis: Heparin is used during dialysis procedures to prevent clotting in the dialysis circuit and maintain the patency of the dialysis catheter.
- Intensive Care: Critically ill patients may receive heparin as part of their care to prevent clot-related complications.
Factors Influencing Heparin Dosage Calculation

The calculation of the heparin drip rate (ml/hr) is a complex process that takes into account several critical factors. Understanding these factors is essential for healthcare professionals to ensure accurate and safe dosage administration.
Patient-Specific Factors
Each patient presents a unique set of characteristics that influence their heparin requirements. These factors include:
- Body Weight: The patient's weight is a key determinant in heparin dosage calculation. Typically, the dosage is based on a weight-based protocol, with adjustments made for patients who are underweight or overweight.
- Age: Age can impact the metabolism and clearance of heparin, requiring dosage adjustments for pediatric and geriatric patients.
- Renal Function: Heparin is primarily eliminated through the kidneys. Patients with renal impairment may require reduced dosages to prevent accumulation and potential toxicity.
- Heparin Sensitivity: Some patients may have increased sensitivity to heparin, requiring careful monitoring and potential dosage adjustments.
- Medical History: Previous exposure to heparin, anticoagulant medications, or bleeding disorders can influence the dosage and administration protocol.
Treatment Objectives
The therapeutic objective of heparin therapy guides the dosage calculation. Different treatment goals require varying heparin concentrations in the bloodstream. The objectives can be categorized as:
- Prophylactic: This objective aims to prevent the formation of blood clots in patients at risk. The dosage is typically lower compared to therapeutic objectives.
- Therapeutic: Therapeutic heparinization aims to treat existing blood clots or prevent their extension. Higher dosages are often required to achieve the desired anticoagulation effect.
Formulation and Delivery Method
The formulation of heparin and the method of delivery can impact the dosage calculation. Heparin is available in different formulations, including unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH). The choice of formulation and delivery method (e.g., intravenous or subcutaneous) can influence the bioavailability and pharmacokinetics of heparin, affecting the calculated dosage.
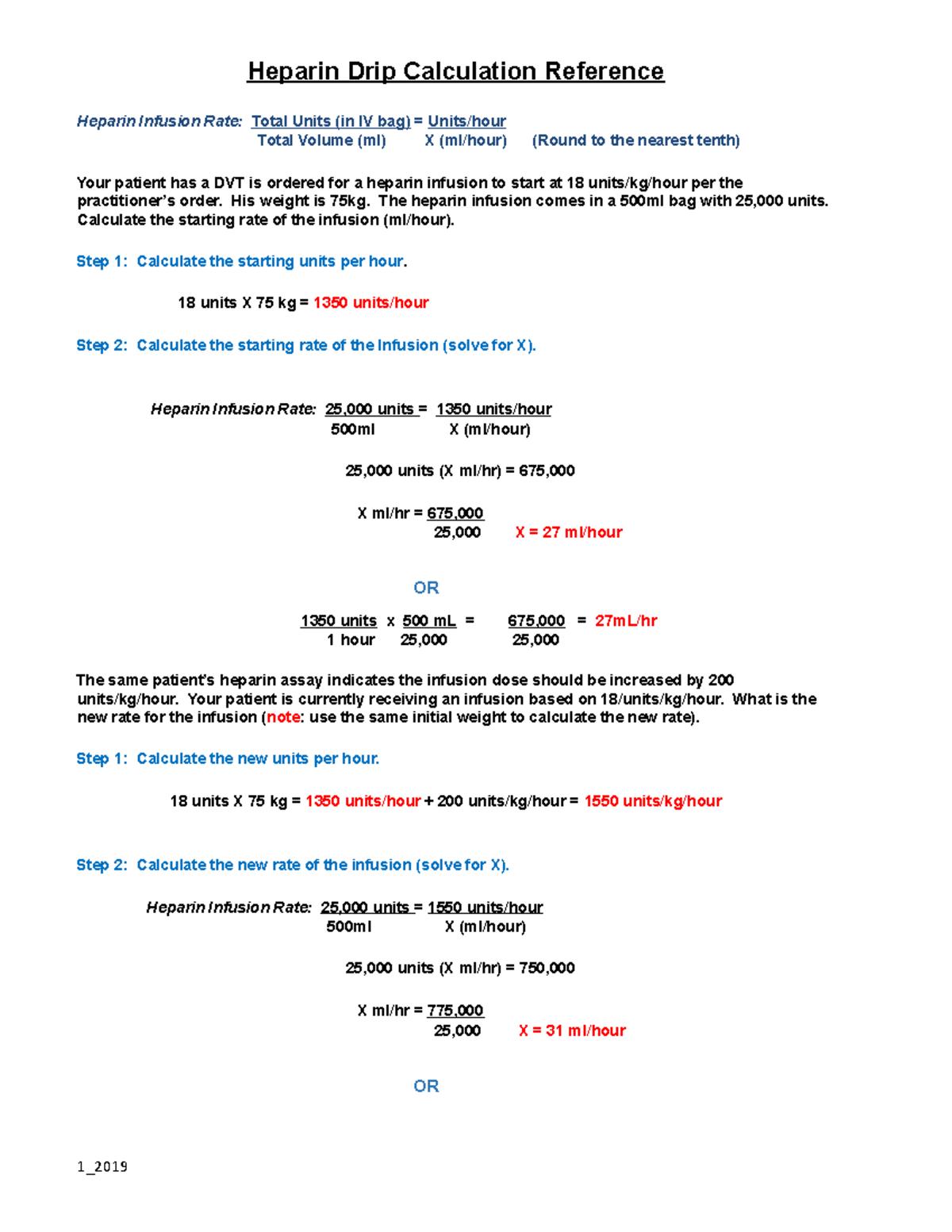
Step-by-Step Guide to Calculating Heparin Drip Rate (ml/hr)
The following is a detailed, step-by-step guide to calculating the heparin drip rate for a typical patient scenario. This example illustrates the practical application of the factors discussed earlier.
Step 1: Assess Patient Characteristics
Gather and review the patient’s relevant medical information, including:
- Body weight: Let's assume the patient weighs 70 kg.
- Age: The patient is 45 years old.
- Renal function: The patient has normal renal function, with no known impairment.
- Medical history: The patient has no known bleeding disorders or previous exposure to heparin.
Step 2: Determine Treatment Objective
Based on the patient’s medical condition, the treatment objective is determined. Let’s assume the patient requires prophylactic heparinization following a surgical procedure.
Step 3: Choose Heparin Formulation and Delivery Method
The healthcare team decides to use unfractionated heparin (UFH) for this patient, delivered intravenously through a heparin drip.
Step 4: Calculate Initial Heparin Dosage
Using a standard weight-based protocol, the initial heparin dosage is calculated as follows:
| Body Weight (kg) | Initial Heparin Dose (IU) |
|---|---|
| 70 kg | 5,000 IU |

Note: The initial dose may vary based on institutional protocols and patient-specific factors.
Step 5: Determine Maintenance Heparin Dosage
The maintenance heparin dosage is calculated to maintain the desired anticoagulation effect. This step involves monitoring the patient’s coagulation status through laboratory tests, such as the activated partial thromboplastin time (aPTT) or anti-Xa activity.
Assuming the patient's aPTT is within the therapeutic range, the maintenance dosage is calculated as follows:
| Body Weight (kg) | Maintenance Heparin Dose (IU/hr) |
|---|---|
| 70 kg | 1,000 IU/hr |
Step 6: Convert Dosage to Drip Rate (ml/hr)
The maintenance heparin dosage (IU/hr) needs to be converted to the drip rate (ml/hr) to set the infusion pump. This conversion depends on the concentration of the heparin solution being used.
Let's assume the heparin solution has a concentration of 10,000 IU/ml. The calculation is as follows:
Maintenance Heparin Dose (IU/hr) / Concentration (IU/ml) = Drip Rate (ml/hr)
In this case:
1,000 IU/hr / 10,000 IU/ml = 0.1 ml/hr
So, the calculated heparin drip rate for this patient is 0.1 ml/hr.
Monitoring and Adjusting Heparin Therapy
Accurate calculation of the heparin drip rate is just the beginning of ensuring safe and effective therapy. Continuous monitoring and adjustment are crucial to maintain the desired anticoagulation level and prevent complications.
Monitoring Parameters
Healthcare professionals should closely monitor the following parameters to assess the patient’s response to heparin therapy:
- Coagulation Tests: Laboratory tests like aPTT or anti-Xa activity provide insights into the patient's anticoagulation status.
- Bleeding: Regular assessment of the patient for signs of bleeding is essential. Heparin therapy can increase the risk of bleeding, especially in certain patient populations.
- Thrombocytopenia: Heparin-induced thrombocytopenia (HIT) is a rare but serious complication. Monitoring platelet counts is crucial to detect this condition early.
- Clinical Response: Evaluating the patient's clinical status, including the resolution of clot-related symptoms, is an important aspect of monitoring.
Adjusting the Heparin Dose
Based on the monitoring parameters and the patient’s response to therapy, healthcare professionals may need to adjust the heparin dose. This can involve:
- Increasing the Dose: If coagulation tests indicate sub-therapeutic levels, the dose may be increased to achieve the desired anticoagulation effect.
- Decreasing the Dose: Conversely, if the patient exhibits signs of over-anticoagulation or bleeding, the dose may need to be reduced to prevent complications.
- Discontinuing Therapy: In certain situations, such as the development of severe bleeding or the resolution of the underlying clotting disorder, heparin therapy may be discontinued.
Potential Risks and Complications of Heparin Therapy

While heparin is a valuable therapeutic agent, it is not without risks. Healthcare professionals must be aware of the potential complications associated with heparin therapy to ensure patient safety.
Bleeding
Heparin’s anticoagulant properties increase the risk of bleeding. Patients receiving heparin therapy should be closely monitored for signs of bleeding, including:
- Unusual bruising
- Excessive bleeding from minor cuts or wounds
- Blood in urine or stool
- Nosebleeds
- Excessive menstrual bleeding
Heparin-Induced Thrombocytopenia (HIT)
HIT is a rare but serious complication of heparin therapy. It occurs when the patient develops antibodies against heparin, leading to a decrease in platelet count and an increased risk of thrombosis.
Symptoms of HIT may include:
- Thrombosis (blood clots)
- Thrombocytopenia (low platelet count)
- Fever
- Rash
If HIT is suspected, immediate discontinuation of heparin therapy and initiation of alternative anticoagulant therapy are necessary.
Other Complications
Other potential complications of heparin therapy include:
- Hypotension (low blood pressure)
- Nerve damage (especially with prolonged use)
- Allergic reactions
- Heparin-induced osteoporosis (long-term use)
Best Practices for Safe Heparin Administration
To ensure the safe and effective administration of heparin, healthcare professionals should adhere to the following best practices:
- Accurate Calculation: Always calculate the heparin dosage and drip rate accurately, following institutional protocols and considering patient-specific factors.
- Close Monitoring: Regularly monitor the patient's coagulation status, bleeding risk, and clinical response to heparin therapy.
- Individualized Care: Tailor the heparin therapy to each patient's unique needs, taking into account their medical history, renal function, and sensitivity to heparin.
- Continuous Education: Stay updated on the latest guidelines and research related to heparin therapy to provide the best possible care.
- Team Collaboration: Ensure effective communication and collaboration among the healthcare team to optimize patient care and safety.
Conclusion
The heparin drip is a critical component of anticoagulation therapy, and accurate calculation of the ml/hr dosage is essential for patient safety and optimal therapeutic outcomes. By understanding the factors that influence heparin dosage, following a step-by-step calculation process, and implementing best practices, healthcare professionals can ensure the safe and effective administration of heparin therapy.
FAQ
How often should coagulation tests be performed during heparin therapy?
+The frequency of coagulation tests, such as aPTT or anti-Xa activity, depends on the patient’s clinical condition and the healthcare institution’s protocols. Typically, tests are performed more frequently during the initial phases of therapy and less frequently once a stable therapeutic level is achieved. For patients on long-term heparin therapy, coagulation tests may be conducted at regular intervals to monitor the patient’s anticoagulation status.
What are the signs of over-anticoagulation with heparin therapy?
+Signs of over-anticoagulation with heparin therapy may include excessive bleeding, such as prolonged bleeding from minor wounds or easy bruising. Laboratory tests may also indicate prolonged aPTT or elevated anti-Xa activity levels. If over-anticoagulation is suspected, healthcare professionals should consider adjusting the heparin dose or exploring alternative anticoagulant therapies.
Can patients with renal impairment receive heparin therapy safely?
+Patients with renal impairment may require adjustments to their heparin dosage to prevent accumulation and potential toxicity. Healthcare professionals should closely monitor these patients and consider alternative anticoagulant therapies if heparin is not suitable. Low-molecular-weight heparin (LMWH) may be preferred in some cases due to its predictable pharmacokinetics in renal impairment.